
Pharmacy Obligations re stolen drugs
The riots in NYC in early June affected many pharmacies. Pharmacy owners felt shocked at the very sight of their looted pharmacies.
Pharmacy benefit management (“PBM”) companies serve as the middle men between insurance companies, drug manufacturers, and independent pharmacies. Four PBMs control 85% of all prescription drugs. By controlling the market, PBMs can choose which drug manufacturers’ medicines will be delivered to pharmacies based on the drugs PBMs reimburse. PBMs then make money by negotiating separate deals with manufacturers, keeping rebates which are meant to be passed to the consumers. They also privately contract with pharmacies and are responsible for paying pharmacies for medications dispensed to patients. PBMs profit by keeping the difference between what the insurance company pays and the funds to meant to pay the pharmacies for medication dispensed to patients. Originally, PBMs promised to keep health care costs low, they have over time merged with big pharmacy chains, made enormous profits, and have taken public funds dedicated for patient care directly for themselves.
In order to combat this problem and encourage more transparency, the New York State Senate passed provision § 280-a of Bill S6531. This bill states that health plan providers are entitled to have access to PBM’s financial information, and PBMs must now disclose any contracts that pertain to the health plan providers. They must also disclose any activity, policy, practice, contract or arrangement they partake that presents any conflict of interest with an associated health plan or provider.
The new regulation states that health care providers or covered patients may be considered third-party beneficiaries of the duties, obligations, and requirements under the pharmacy benefit manager. This entitles them to legal or equitable relief in case of violation of said duties, which means that PBMs now have a duty of care directly to patients and pharmacies. Additionally, PBM’s do not have the right to substitute or alter a prescription drug without the proper authorization of a licensed professional who deals with such matters, simply PBMs can no longer intervene and only pay for a generic.
PBM’s must now be licensed. Licenses are granted through state superintendents based on trustworthiness, competency, and completion of any pre-requisite. Superintendents may also refuse to renew licenses if PBMs have shown signs of untrustworthiness, such as withholding money, being financially irresponsible, or being dishonest. PBMs may also have their licenses revoked for the aforementioned reasons, as well as informed misrepresentation and fraudulent behavior in regards to their professional duties.
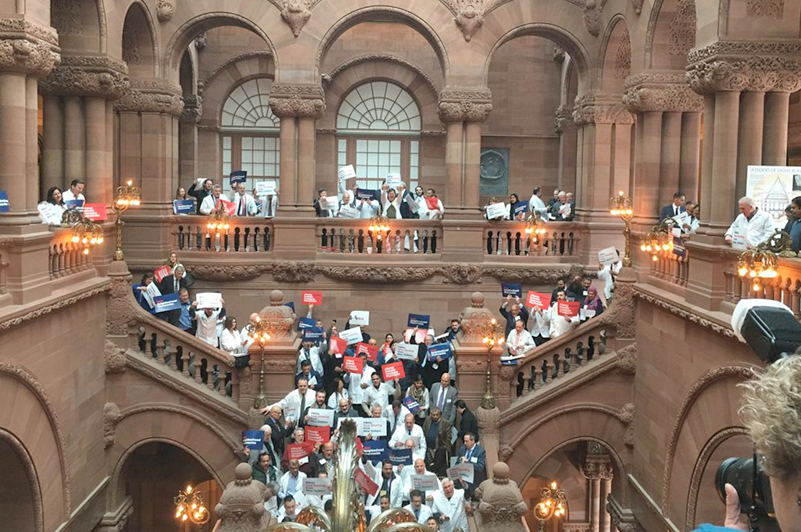
These new regulations were passed in large part due to the lobbying efforts of the Pharmacy Society of the State of New York (“PSSNY”), which invited SAPG Legal to join in those lobbying efforts in Albany earlier this year. The regulations protect consumers and drug manufacturers, as well as allowing independent pharmacies to survive. It makes the business of selling medicine more transparent for each entity on either side of the business.

The riots in NYC in early June affected many pharmacies. Pharmacy owners felt shocked at the very sight of their looted pharmacies.

Commercial litigation can be quickly resolved in a settlement or end up going to trial which may take as long as 3 years!

SAPG Legal Attorney Steve Polyakov discusses how long a Pharmacy can close before causing any issues with the New York State Board of Pharmacy.

When selling your business focus on whether your selling your company as a whole or assets of the company, decide whether there will be financing
SAPG is a client-centred international law firm with a custom-tailored approach.